Sleep disordered breathing
The term ‘sleep disordered breathing’ refers to a range of conditions that result in abnormal breathing during sleep. The most common is sleep apnoea. Apnoea means a temporary pause in breathing. Although there are other types of apnoea, the term ‘sleep apnoea’ usually refers to obstructive sleep apnoea syndrome (OSAS) in which the individual is briefly unable to breathe due to temporary obstruction of the airway in the throat, called the pharynx. In patients with OSAS this may occur many hundreds of times during a single night’s sleep.
Symptoms
When we are asleep, our muscles are relaxed. In some people, the tongue and the relaxed muscles in the throat can cause a narrowing of the airway, which restricts breathing and can stop it temporarily. If this happens, the brain causes brief partial awakening, which reopens the airway and restarts breathing. Repeated awakenings in the night can seriously affect the quality of sleep, leading to excessive daytime sleepiness.
In addition, each apnoea is accompanied by a surge in heart rate and blood pressure. Eventually the increased blood pressure (hypertension) persists even when awake and this increases the risk of a heart attack or a stroke. OSAS is also associated with an increased risk of diabetes, memory issues and dementia.
Snoring is universal in people with OSAS. The noise of snoring arises from vibration of the tissues in the throat, implying that the airway is potentially unstable and therefore more vulnerable to collapse during sleep. However, only a minority of snorers have OSAS.
Symptoms of OSAS can occur both day and night:
Day
- Excessive sleepiness
- Lack of concentration
- Morning headache
- Changes in mood
- Dry mouth
- Impotence or a decreased sex drive
Night
- Restless sleep
- Apnoeas
- Awaking with choking
- Vivid dreams
- Nocturia (urination at night)
- Sweating
- Insomnia
- Salivating and teeth grinding
Causes
The prevalence of sleep apnoea increases with age up to 60 years.
Anything causing the throat to be narrower than average can increase the likelihood of OSAS because it makes it easier for the airway to collapse when breathing in. Other factors, such as how the body controls breathing and how easily someone wakes up, can also make the airway more likely to collapse.
Environmental factors
These are external factors or lifestyle choices that can contribute to OSAS and may be managed:
- Moderate or severe obesity is a major risk factor as it is accompanied by an increase in the fatty tissue around the throat. Obesity is found in between 60 and 90% of people with OSAS and is the most common risk factor in adults.
- Smoking and alcohol have both been linked with a higher prevalence of snoring and sleep apnoea.
- Nasal congestion: Severe congestion of the nose, whether from allergies or other issues, can make breathing difficult and worsen OSAS, especially in children.
Genetic factors
Some people are more likely to develop sleep apnoea because of their genes.
- Sleep apnoea is more common in men than women.
- Certain types of inherited facial bone structure are associated with a narrow throat and make OSAS more likely; the commonest is a receding chin. Specific genetic conditions such as Down syndrome also predispose the individual to OSAS.
- OSAS also occurs in children and the commonest contributory factor is enlargement of the tonsils. In some children or adults severe congestion of the nose can make the condition worse.
- Tonsils and adenoids: OSAS also occurs in children and the commonest contributory factor is enlargement of the tonsils and adenoids. The adenoids are small pieces of tissue behind the nose that can become enlarged and block the airway, making breathing difficult.
- Breathing control issues: Some people may inherit traits that affect how the brain regulates breathing during sleep, making them more prone to unstable breathing patterns. However, non-genetic factors such as age, medications or other health conditions can also affect breathing control and contribute to OSAS.
Prevention
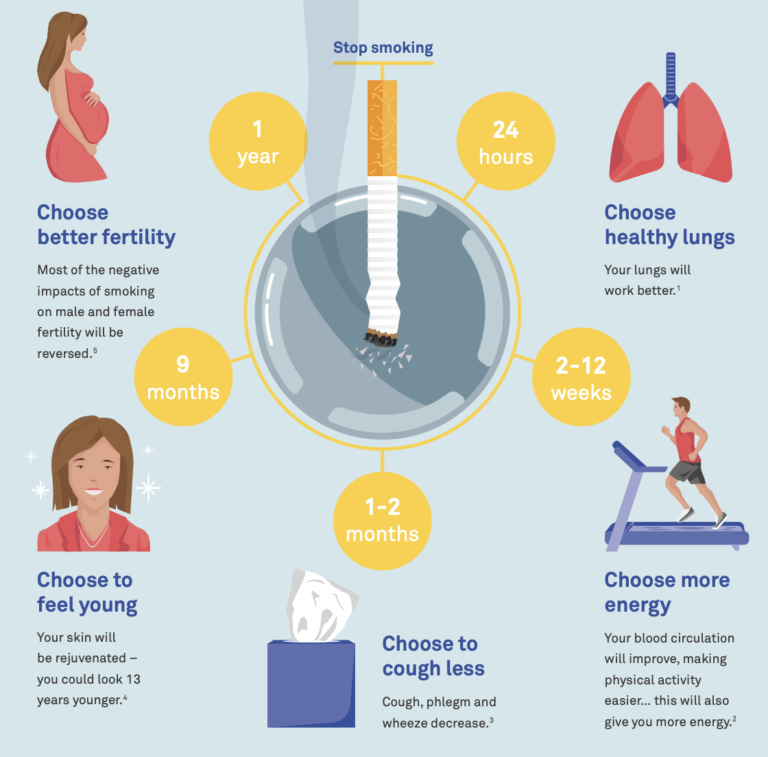
Where relevant, lifestyle changes such as weight loss and reducing alcohol consumption and cigarette smoking can all help prevent the condition.
Additionally, maintaining adequate sleep hygiene, such as consistent sleep schedules and avoiding stimulants before bedtime, may be beneficial.
Diagnosis
OSAS is often suspected from symptoms and clinical examination but in most cases overnight recording is needed for confirmation. A detailed sleep study, called polysomnography, records brain waves, muscle activity, eye movements, heart activity, chest movement, airflow at the nose and mouth and blood oxygen level (oximetry).
This detailed study is carried out in in a sleep clinic but with most individuals with suspected OSAS, simpler investigations can be performed using portable equipment, often in the patient’s home. Several devices are now available to record various combinations of blood oxygen levels, chest movement, airflow and heart rate. This includes homes sleep apnoea testing (HSAT), which uses polygraphy, also known as cardiorespiratory monitoring. This is a simpler test that records important information about breathing and heart function during sleep.
The level of daytime sleepiness is assessed by a simple questionnaire called the Epworth Sleepiness Scale. This asks the individual to grade the likelihood of falling asleep in different everyday situations. Symptoms of sleep apnoea such as snoring and witnessed apnoeas are also likely to be reported by a bed partner.
Treatment
The most effective treatment for sleep apnoea is continuous positive airway pressure (CPAP), which is simple and highly cost effective. This form of treatment involves a machine which generates a flow of air via a mask over the nose (or nose and mouth) at a pressure which is adjusted to keep the throat open during the night. For continuing benefit it needs to be used every night.
Other options include:
- Mandibular advancement devices (MAD) are mouthpieces worn over the teeth. These are worn inside the mouth to bring the lower jaw forward and help keep the airway open. This treatment is most effective for snoring and may be recommended for mild OSAS or for people with more severe cases who cannot tolerate CPAP.
- Positional and myofunctional therapy works to improve the muscles in your throat and mouth. Positional therapy promotes sleeping in positions that help keep the airway open, such as avoiding sleeping on your back. Myofunctional therapy involves doing exercises that strengthen the muscles around your mouth, throat and tongue to help prevent blockages while you sleep. These treatments are usually recommended as supplementary options.
- Surgery is rarely a primary treatment option in adults unless there is a clear obstruction, such as enlarged tonsils, which is more common in children. Other procedures that involve removing parts of the throat to create more space have largely been abandoned due to limited effectiveness.
New research is exploring new drugs to treat moderate to severe OSAS but while these treatments show promise for the future, drug treatment is not currently a recognised option for managing OSAS in clinical practice.
This page was updated in 2025.
ERS Sleep and Breathing Conference 2021: Lay summaries of key sessions chosen by patient representatives
In April 2021, the European Respiratory Society (ERS) held a virtual conference on sleep and breathing disorders. Members of the ELF Sleep Patient Advisory Group (PAG) chose the conference presentations that they were most interested in, and we have prepared lay summaries of those presentations.
Access the lay summariesIf you want to access data on sleep apnoea in Europe, visit the Lung Facts website
Launched by the International Respiratory Coalition and using data from the Global Burden of Disease study, Lung Facts provides the latest numbers on people living with lung disease by condition and by country.
Learn more